Mpox Resource Center
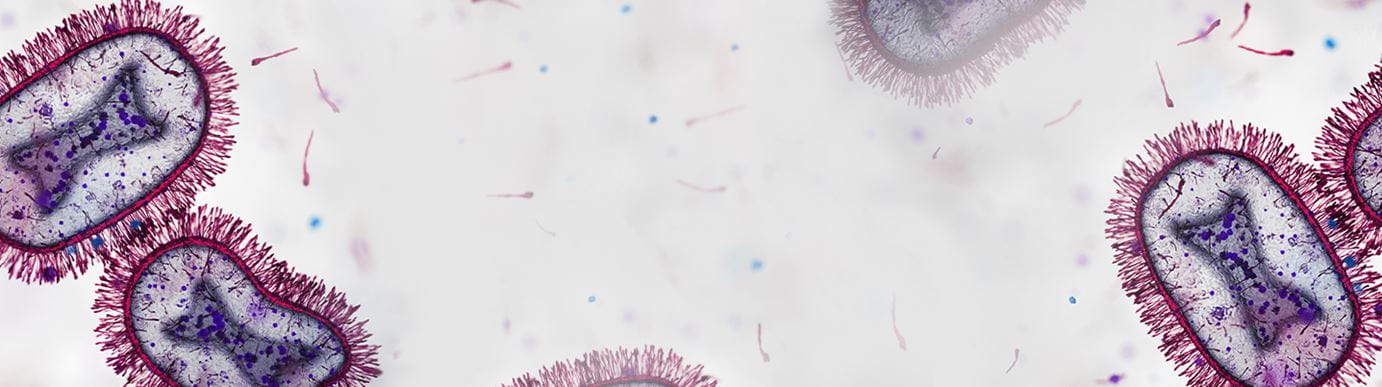
Mpox, the disease formerly known as monkeypox, has been declared a global health emergency for the second time in two years by the World Health Organization, following a spike in cases in a growing number of countries in Central and West Africa. Learn more on our blog.
While the current risk for most people in the U.S. is low, the disease still circulates in small clusters.
If you've been in close contact with someone who has mpox or suspect you may have mpox, Houston Methodist offers three convenient options to see a provider for advice, testing and medical care:
- You can make a virtual appointment with your primary care physician (PCP). If you do not have a primary care physician, call 346.356.3102.
- You can make an appointment online at a Houston Methodist Same Day Clinic or call 832.730.0194.
- You can see a provider virtually via Virtual Urgent Care, available 24/7 or download the MyMethodist app.
In addition, you should pre-emptively try to self-isolate, wash your hands frequently and avoid close contact with others.
Last updated October 19, 2024