Decoding COVID-19: The Delta Variant, Vaccines & Other Trends We're Tracking
July 28, 2021 - Eden McCleskeyA month ago, Alpha was topping the charts. Today, the Delta variant reigns supreme as we wait to see what the upstart Lamba has up its sleeve. It sounds like a bad reality TV concept. American Ninja Warrior meets The Voice meets the Indy 500. As weary followers of the COVID-19 drama for nearly 18 months now, it's tempting to write off the latest twists and turns of various variant contenders as irrelevant subplots or desperate ratings gambits.
Unfortunately, this is not a fantasy, and it's nobody's idea of entertainment. Which means there are important reasons why we're hearing about the Delta variant so much, and instructive information to be gleaned from the unprecedented real-time genetic tracking of COVID-19 and its many variants.
To help us break down the lessons learned so far — and put it in perspective for clinicians wondering what to tell their patients next — two Houston Methodist experts, Dr. Randall Olsen, professor of clinical pathology and genomic medicine, and Dr. Wesley Long, associate professor of clinical pathology and genomic medicine, sit down to discuss their ongoing efforts to sequence the genome of every COVID-19 positive test in the Houston Methodist system.
Their most recent study, analyzing trends from more than 12,000 SARS-CoV-2 virus genomes sequenced in 2021, was recently published in the American Journal of Pathology.
Tell us about the background of this study. How did it come about?
Dr. Long: We have a track record of sequencing large, comprehensive, population-based genomic datasets of pathogens. Prior to COVID-19, we were studying group A streptococcus, staphylococcus aureus, klebsiella, lots of different bacteria. We would usually work retrospectively, several months or years of specimen collections sequenced all at once then analyzed.
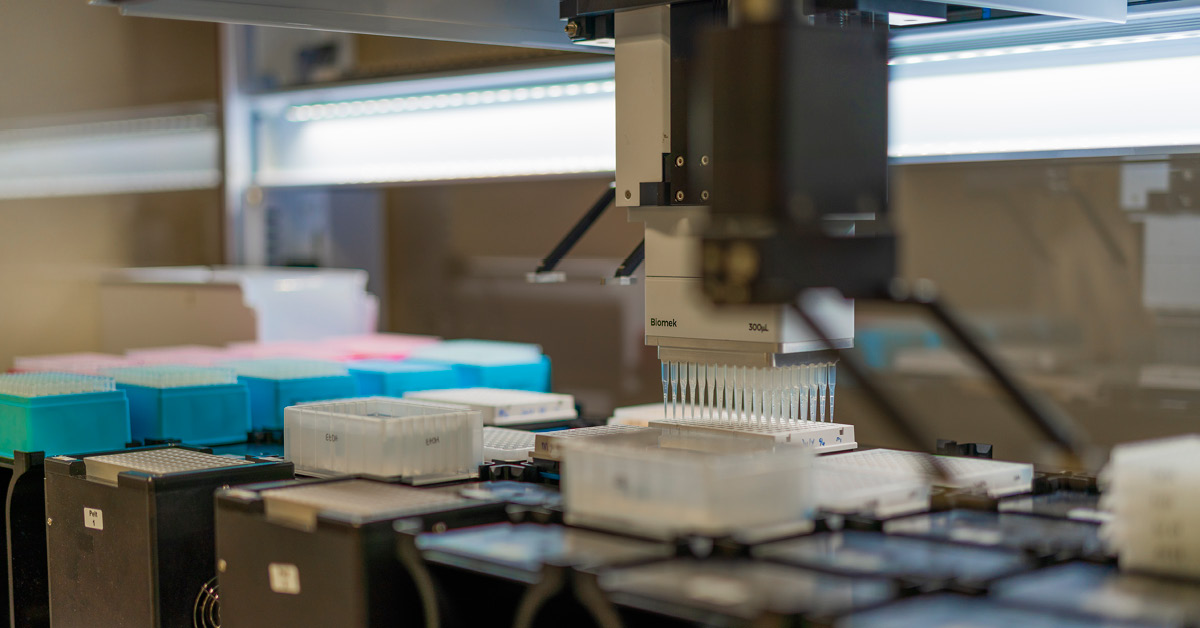
Dr. Olsen: This kind of large-scale sequencing operation is a technically very complicated process, particularly the bioinformatics anaylsis. There were very few places in the U.S., or the world, that were prepared to rapidly implement COVID-19 sequencing at this scale. We already had most of the infrastructure and the preexisting pathogen genomic expertise, so we were able to adapt it quickly for COVID-19.
Dr. Long: In January 2020, when we identified that this was going to be a globally significant pathogen, we started putting together everything we needed to test for COVID-19, before commercial tests were available, and started putting together a plan to sequence it. We knew that the genomic information was going to be very useful for public health monitoring, and initially to see where the cases were coming from, so we could brace the health care systems appropriately. As the pandemic went on, and vaccines began to roll out, the focus shifted to looking at the clinical implications of new mutations (and new variants) and the potential for vaccine or therapeutic escape.
Dr. Olsen: By identifying the mutations as they're occurring in our patients, it helps us make predictions on things like the severity of the disease course, or the effectiveness of monoclonal antibody therapies and vaccines.
How are you able to make clinical predictions just from reading the genome of the virus?
Dr. Long: It's because we have both the lab capabilities and the clinical information that comes along with being a large academic medical center. We have their entire clinical history, because they were our patients. We know their health histories, where they live, if they went into the hospital with COVID-19, how long they stayed, whether certain treatments were effective.
Dr. Olsen: It's definitely something that sets us apart — to have integrated virus genome and patient data. Another unique aspect of our operation is the catchment of the Houston Methodist system. We cast a large net across the entire metro area, so our data is generally representative of infections throughout the metroplex.
Dr. Long: We can track hot spots in Houston, and test hypotheses, such as whether certain variants of concern are causing breakthrough infections at higher rates. Sometimes variants hit Europe or other parts of the world first, and there are reports that it's more contagious or more severe. We can check that against our own patient data to see if this specific variant causes more hospitalizations or longer hospital stays. And, as we get larger and larger sample sizes, we can see that maybe no, in fact, it doesn't cause more severe illness here in Houston. Or, yes, it does still respond to the monoclonal antibody therapies. And that helps everybody improve outcomes.
Dr. Olsen: We are continuously reanalyzing the entire data set with our clinical information attached to it. It gives us a really powerful tool to make associations between the genetics and the disease phenotypes.
How do you know when a variant is going to be significant or 'of concern'?
Dr. Long: There's a lot of variation, a lot of random mutations, in all the individual viruses we sequence. It's whenever some set of mutations becomes advantageous, and we start to see it become dominant. The first one was D614G, which swept through Europe and then the U.S. in Spring/Summer 2020. There was a single change in the spike protein from the original virus, and it enhanced transmissibility. The next big one, the Alpha variant from the U.K., showed up originally in December 2020. Again, that one got everybody's attention because it was more transmissible and swept through the U.K., Europe and other places worldwide. Sometimes a cluster of the same mutations appears and then it just dies out. There was one variant in Singapore that caused notably less severe illness. But it also didn't spread as well, so it never really caught on.
Dr. Olsen: New variants are constantly developing. Some of them are going to be dead ends. But some of them have an advantage that will allow them to successfully spread and cause severe disease, like we're seeing now with the Delta variant. It's sort of what viruses do, and an important part of why we continue doing the research. We must detect that next variant early so that we can guide public health maneuvers.
So, besides enhanced transmissibility, do the variants keep getting worse?
Dr. Olsen: We know that statistically the Delta variant, compared to other variants, causes more severe disease and more hospitalizations.
Dr. Long: Now that we have vaccines, there's a lot of concern about whether we are going to get a variant that's going to render the vaccines less effective. That's a big concern. So far, the evidence shows that almost all new infections, including those with the Delta variant, occur in unvaccinated people. This really strongly underscores the need to continue vaccination efforts.
Dr. Olsen: If you are not yet vaccinated, now is the time.
Is there something inherent about Delta that is making people more worried about it?
Dr. Olsen: Our big concern about Delta is that it's going to cause another surge due to its enhanced transmissibility, similar to what occurred in the U.K.
Dr. Long: Really, Delta arrived in the U.K. and the U.S. at the same time. But the U.K. had a lower percentage of people fully vaccinated. They prioritized getting everyone the first shot, while we prioritized giving those who qualified for it both shots. So, it moved into the U.K. and swept in a month, whereas in America, it's been much more of a slow burn. But now, Delta has become the most common cause of infections in our patients.
What is the most important thing that you want your colleagues to take away from your research tracking these variants?
Dr. Olsen: Vaccinate. Vaccinate. Vaccinate.
Dr. Long: The key to emerging from the pandemic is getting more people vaccinated.
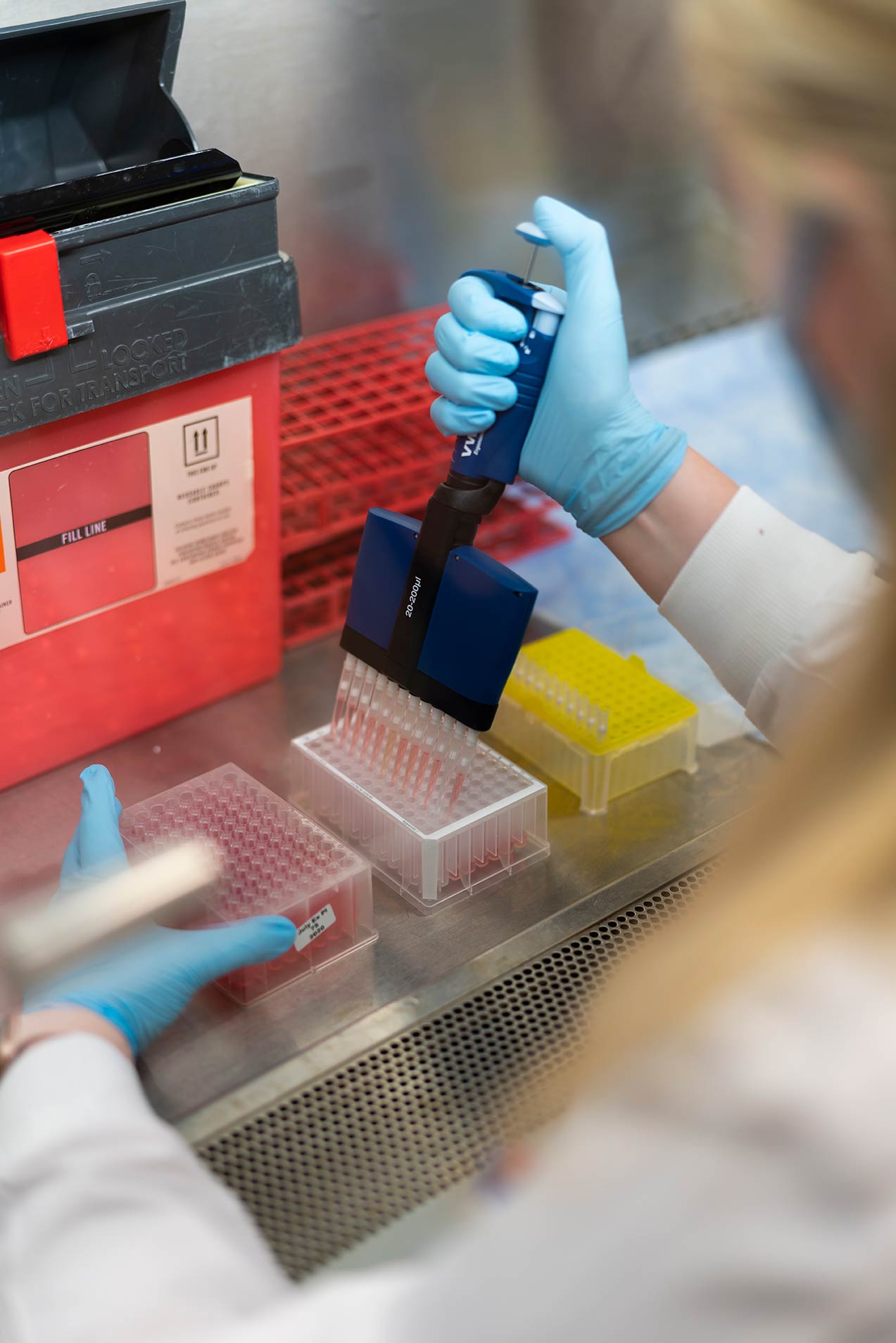
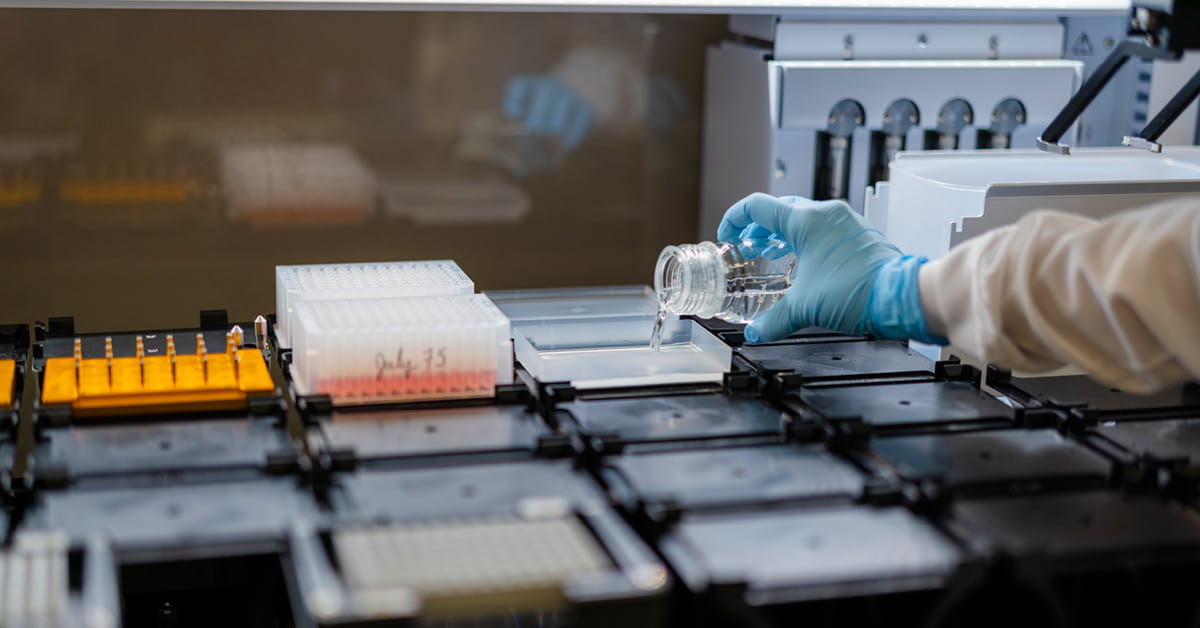
Scenes from the lab
The COVID-19 genomics team at the Houston Methodist Research Institute includes Akansha Batajoo, Jessica Cambric, Ryan Gadd, Regan Mangham, Matthew Ojeda Saavedra, Sindy Pena, Layne Pruitt, Kristina Reppond, Madison Shyer and Rashi Thakur.