Diagnosis & Management of ALS
Diagnosing ALS is difficult in early stages because it presents many of the same symptoms as other neurological conditions; however, a medical history, physical examination and neurological examination are typically enough to suggest the diagnosis of ALS.
In an electromyogram (EMG), a needle will be inserted into various muscles to evaluate the muscle’s electrical activity at rest and in contraction. Various abnormalities may be detected, including small involuntary muscle contractions (fibrillations), positive sharp waves, a reduction in the number of voluntary motor units and spontaneous muscle twitches (fasciculations). Remaining healthy motor neurons can reinnervate muscles and EMG can highlight this process. Single-fiber EMG tests may show decreased fiber densities as an example of reinnervation.
A nerve conduction velocity study will measure the nerves’ ability to send impulses to other parts of the body in order to test for nerve damage. In ALS, the speed with which the impulse travels is usually normal, but there may be slight slowing; if slowing is greater than expected, the cause may be from a neurological condition other than ALS. An MRI will produce detailed images of the brain and spinal cord to look for lesions or tumors that may be causing the symptoms. Blood and urine tests may help to rule out other possible causes for the symptoms. High resolution serum protein electrophoresis can rule out ALS-like conditions associated with abnormal proteins secreted by plasma cells (monoclonal gammopathy). If this condition is suspected, a bone marrow biopsy may be required. Measuring thyroid hormone levels helps to exclude the forms of hyperthyroidism that mimic ALS with muscle weakness, wasting, muscle twitches and increased reflexes. Neuromuscular symptoms may be present due to hyperparathyroidism hormone levels and cause weakness, fatigue and increased reflexes. A spinal tap (or lumbar puncture) may be used to remove a sample of spinal fluid which will be analyzed. A muscle biopsy may be used to eliminate a muscle disease as the cause of symptoms.
Monique Green's Story
Monique Green is a nurse practitioner; who works with HIV patients. She sees the challenges these patients face and sometimes compares their challenges to her own.
Managing ALS
No cure for ALS exists and the progression of the disease cannot be reversed, so treatment focuses on slowing the progression of symptoms, avoiding unnecessary complications and making the patient as comfortable and independent as possible. The disease involves the complex interaction of physical, mental and emotional issues, so the integrative, multidisciplinary team approach at Houston Methodist is essential in prolonging survival and improving quality of life.
The drug riluzole may be recommended to help slow the progression of ALS; it works in some people by possibly reducing the levels of the neurotransmitter glutamate in the brain.
Exercise and lifestyle modifications are critical to managing the symptom of muscle weakness.
Regular, individualized exercise programs (never to the point of exhaustion) have been shown to slow muscle wasting in people with ALS and minimize spasticity. Recommended exercises include stationary bicycle riding, walking on even surfaces and water exercises (but not weightlifting or resistance training).
Adaptive devices designed for specific limb weakness can help improve a patient’s independence. For example, an ankle-foot orthotic can help to minimize falls and maximize endurance. Splints can be used to increase grip strength and improve finger dexterity and button hooks, zipper pulls and larger-handled utensils can make daily tasks easier.
Modifying bathrooms and other sites in the home, as well as using walking devices such as cane, walkers and wheelchairs, can help eliminate falls due to muscle weakness.
Muscle weakness can place excessive stress on joints, as can the pressure from prolonged sitting or reclining. Anti-inflammatory medications, frequently changing position, stretching exercises and specialty mattresses can help reduce pain.
Medication is also an option to relieve some of the symptoms of ALS:
- Cramps and spasms
- Spasticity
- Constipation
- Fatigue and general muscle pain
- Depression
- Problems sleeping
- Uncontrollable outbursts of laughing or crying (known as pseudobulbaraffect)
- Increased saliva or phlegm
Several therapy options may be of help in managing ALS:
- Physical therapy to help maintain muscle strength and flexibility and help the patient transition to devices to help with mobility
- Occupational therapy to help the patient compensate for hand and arm weakness and to modify the home
- Speech therapy to help make speech better understood and to introduce devices to aid in communication
- Breathing care to introduce devices to help the patient breathe as muscles become weaker
Slurred speech in ALS patients can be frustrating, but numerous devices can help a person communicate (from computer tablets to a simple “magic” slate erasable writing pad). A speech pathologist can assist the patient to find the best option to achieve the goal.
Therapy for respiratory dysfunction is intended to provide general breathing support:
- Careful monitoring of breathing
- Promptly treating all respiratory infections
- Providing supplemental oxygen if blood oxygen levels are low
- Minimizing the chances of aspiration in patients with swallowing difficulties
- Providing drugs to help decrease excessive saliva or phlegm
- Using suction devices to remove excess secretions
Breathing exercises may help strength diaphragm muscles. Non-invasive machine ventilation (for example, a CPAP machine) can improve breathing.
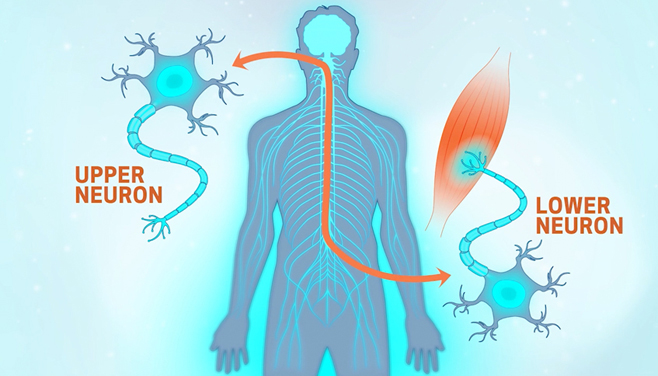
ALS patients may be affected with pseudobulbar affect, inappropriate crying or laughing outbursts associated with upper motor neuron dysfunction which is not an indication of a psychological problem. Medication can help alleviate this condition.
Our team will also assist the patient in engaging nutritional experts to provide foods that meet nutritional needs and are easy to swallow. Generally, no change in diet is necessary with ALS, but swallowing difficulties can make it a challenge to both nourish the body with a balanced meal and to maintain a healthy weight. Some strategies to help patients meet dietary goals include more frequent and smaller meals, as well as the inclusion of high-protein, high-calorie snacks between meals. The addition of a multivitamin and fruits and vegetables (in fresh or juice form) can make it easier to get the required vitamins and minerals.
Since there is a possibility that oxidative stress may contribute to ALS, increasing the amounts of antioxidants such as vitamins E, C and beta carotene may be beneficial. A recent experiment using genetically engineered mice with the same mutated gene that occurs in people with familial ALS shows that adding vitamin E to the food delays the onset of motor neuron loss and oxidative damage and slows progression of the condition, but does not prolong survival.